Start feeling better today!
Connect with your therapist today and take control of your life like our 850.000 happy clients.
Get StartedWhat is Vaginismus?
Vaginismus is the involuntary, repetitive, and continuous contraction of the muscles at the entrance of the vagina just before or during vaginal intercourse, and the feeling of pain due to these contractions. It is associated with negative thoughts, experiences, and reactions to sexuality.
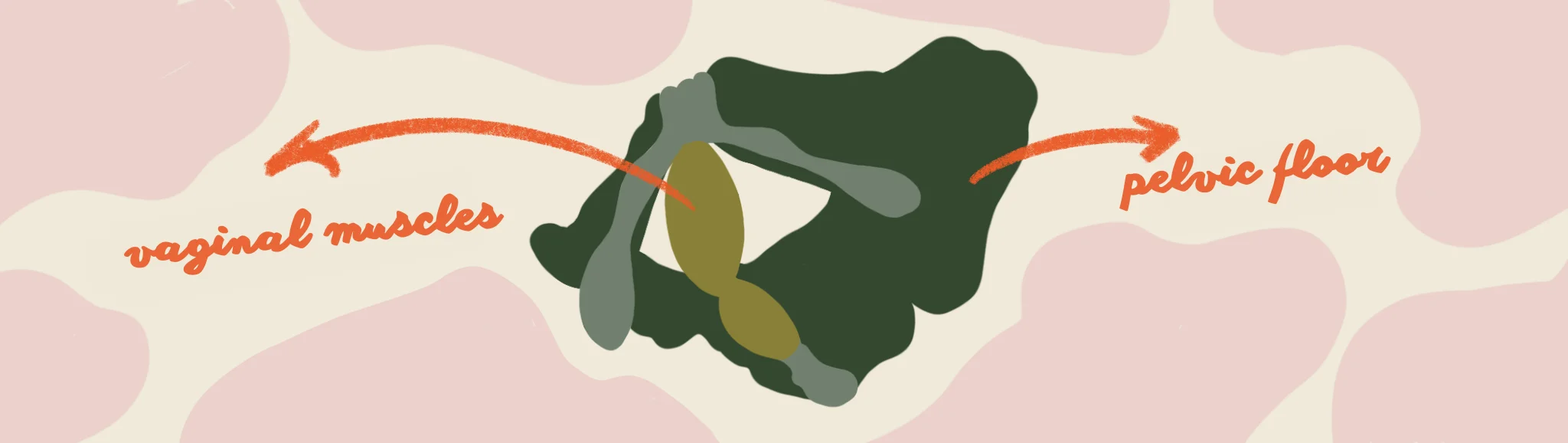
The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) includes vaginismus in the group of genito-pelvic pain and penetration pain disorders. Accordingly, vaginismus causes the person to feel pain in the pelvic floor, vagina, or vulva during any sexual intercourse, use of tampons, use of sex toys, or stimulation of the vagina with fingers.
Although vaginismus is a physical reaction, it is largely triggered by social and environmental factors. In other words, vaginismus is not a problem of vaginal contraction but a problem of contraction of the vagina as a result of misconceptions, fears, and anxieties about sexuality, preventing sexual intercourse or causing painful sexuality.
The relationship between muscles, emotions, thoughts, and pain is often misunderstood. This misunderstanding creates an environment where people who are not experts in the field or who are not authorized and skilled in sexual therapy can take advantage of the situation.
Everyone has the right to accurate and evidence-based support without being duped by so-called experts who exploit information pollution, feelings of discomfort when discussing sexuality, and a lack of systemic support mechanisms. In this article, you can find answers to questions such as what vaginismus is, why it is caused, and how it is treated.
What are the Causes of Vaginismus?
Vaginismus is related to sexual anxieties and fears and can be caused by a combination of many factors. Some of these include:
- Lack of access to reliable sexuality information
- Stereotypical misconceptions about sexuality
- Adverse experiences, violence, and trauma
- Family and social misconceptions
- Pressure from the partner
Lack of Access to Reliable Sexuality Information
Lack of accessible sexuality education, non-judgmental and empowering discussions about sexuality in the family and immediate environment, and a lot of misinformation about sexuality can lead to misconceptions and make people feel alone about their experiences.
Sexuality education can help to understand the sexual organs, the functioning of the body, the mechanisms of pleasure and orgasm, communication, and sharing in relationships. Lack of access to reliable resources can increase uncertainty about sexuality and lead to fear and anxiety.
Stereotypical Misconceptions About Sexuality
Some stereotypical messages about sexuality and sexual intercourse portray sexuality not as something that can be positive, but as something that is expected to be forced, and that the body and virginity must be protected.
These misconceptions can trigger negative feelings and thoughts about sexuality. Some common problematic messages include:
- "It will hurt in sexual intercourse anyway."
- "I'm considered not a virgin if I don't bleed the first time."
- "Sex is for the pleasure of the man."
- "This is my duty."
- "If I don't do it, I'll be dumped."
- "If I masturbate or use tampons, I will lose my virginity."
Adverse Experiences, Violence, and Trauma
Exposure to sexual, physical, or psychological violence, such as sexual harassment, rape, and abuse, can change a person's feelings and thoughts about sexuality and sexual behavior and affect their experiences.
Family and Social Misconceptions
The reactions, attitudes, and messages conveyed by families towards sexuality, the body, relationships, and the building blocks of sexuality such as gender identity and gender expression can have an impact on the perception of sexuality, values, and sometimes anxiety and fears.
When these attitudes are presented in sex-negative ways, that is, as judgmental, frightening, repulsive, and sinful, they can negatively affect people's perceptions of sexuality and put pressure on them.
Pressure from the Partner
Partner's insistence, insisting on sexual behavior or forcing certain sexual behaviors, painful sexual behavior, or ignoring the needs of the other person during intercourse can cause fear, anxiety, disgust, and anxiety about sexual intercourse.
Symptoms of Vaginismus
Some of the symptoms of vaginismus include:
- Failure of vaginal intercourse due to contraction
- Pain in the vulva, vagina, or pelvic floor during vaginal intercourse attempts
- Fear or anxiety about vaginal intercourse and/or the pain it may cause
- Symptoms persisting for at least 6 months
- A significant and involuntary tension and contraction of the pelvic floor muscles during vaginal intercourse
How Common is Vaginismus?
Research shows that vaginismus has an average prevalence of between 1% and 25% worldwide. This range varies depending on factors such as geography, research frequency, and intensity. In Turkey, vaginismus is more common than in many other countries. This underlines the social and cultural causes of vaginismus.
People diagnosed with vaginismus experience fear of sexuality, but this does not mean that everyone with sexual fears will be diagnosed with vaginismus. People diagnosed with vaginismus can sometimes experience painful sexual intercourse, but the painful sexual intercourse experienced by every person may not be vaginismus.
Sometimes hearing non-vaginismus situations from the environment with phrases such as "vaginismus" or "I think I have vaginismus" can cause people to think that vaginismus is much more common than it actually is.
How is Vaginismus Treated?
Vaginismus is a sexual dysfunction. Premature ejaculation, erection problems, and the inability to experience orgasm are some of the sexual dysfunctions. Sexual dysfunctions respond positively and non-recurrently to therapies within a certain period of time.
Vaginismus can also be treated with the support of psychiatrists and clinical psychologists who have received the necessary training and can perform sexual therapy.
Although physicians, sociologists, sexuality educators, and other professionals working on sexuality can provide information to raise awareness about vaginismus, they cannot intervene to treat vaginismus. One of the main reasons for this is that vaginismus is a defined dysfunction related to human psychology that can be addressed through sexual therapy.
Vaginismus and Sexual Therapy
Sexual therapy for vaginismus usually involves both partners, but individual therapy is also possible. Sometimes, in addition to couples therapy, vaginismus may also require individual work.
Sexual therapy is verbal and consists of a series of sessions that include sexuality education, addressing beliefs about sexuality, addressing fears and anxieties, and exercises, followed by assessment. Nudity and physical contact are never used during sexual therapy.
As everyone's sexuality, general health, and relational and environmental realities are different and unique, everyone may have different needs in the sexual therapy process. Although it is usually possible to treat vaginismus with consecutive therapy sessions over several months, sometimes it may be necessary to seek longer-term support.
Is the Goal in the Treatment of Vaginismus to Have Intercourse?
Vaginismus is the physical manifestation of a psychological condition, so the goal of its treatment is not only physical. In other words, the goal of vaginismus treatment is not vaginal intercourse. It is to enable the person to experience their sexuality without fear and tension, without pain, without complaints, and in a way that is good for them. Sexual intercourse may be part of the healing process, but it is not the main goal.
Can Gynecologists or Non-Psychiatrist Doctors Treat Vaginismus?
Gynecologists and non-psychiatrists are not physicians who can provide mental health treatment. Gynecologists take an active role in the diagnosis and treatment of physical health problems related to the vulva, vagina, clitoris, labia minora, urinary tract, uterus, and ovaries.
Injury to the external or internal genitals, infections, or other health conditions can also cause pain during sexual intercourse. Therefore, the diagnosis of vaginismus may be preceded by a gynecological examination.
This examination can help determine whether the condition experienced is due to a physical condition. This is also called organic causes. This means that if the person experiencing pain does not have any organic symptoms, it can be concluded that the condition is psychological rather than physical.
Gynecologists, after performing the necessary physical examination, can provide information on whether the complaint is physical or if the symptoms are related to vaginismus. Beyond this, they should not use therapy to cure vaginismus and should refer their clients to a mental health specialist.
Due to the lack of professional law and knowledge in the field of sexuality, sometimes people who are not authorized to provide therapy claim to be able to provide therapy and apply non-evidence-based methods.

How Does Vaginismus Affect Relationships?
How partners handle vaginismus is an important factor in determining how the relationship will be affected. Forcing and insisting on sexual intercourse, not communicating, punishing the partner, expressing anger, and using violence can negatively affect relationship dynamics.
Sharing sexual problems between partners with family members and extended family without the partner's permission can also complicate the process. On the other hand, a supportive and solution-oriented approach can relieve the relationship and the partner experiencing vaginismus.
Can People Diagnosed with Vaginismus Have Sexual Intercourse?
The presence of vaginismus does not mean that a person cannot have sexual intercourse before treatment, because sexual intercourse is not only the penis entering the vagina.
The idea that "real" sexuality can only be experienced through penis-in-vagina intercourse is a misconception that has emerged as an extension of gender roles.
People can be stimulated through many different sexual behaviors, build intimacy with their partner, and experience sexual pleasure and orgasm without intercourse.
Does Vaginismus Prevent Pregnancy?
Vaginismus is a dysfunction that is treatable and can respond to treatment in a relatively short period of time. Therefore, both sexual intercourse and pregnancy can occur after vaginismus treatment.
In addition, vaginal intercourse is not the only condition for pregnancy. Various pregnancy methods offered by modern medicine are always an option.
Definitions of some terms used in the article:
Pelvic floor: It is the layer of muscle and connective tissue formed by the pelvis that enables the uterus, ovaries, and large intestines to perform their functions.
Vagina: It is included in the internal genitals. It is an organ that continues into the inside of the body, with the outer part included in the vulva. It is connected to the uterus by the cervix.
Vaginismus: Involuntary and continuous contraction of the muscles at the entrance of the vagina due to fear and anxiety about sexuality and sexual intercourse and experiencing pain due to this contraction.
Vulva: External genitalia that include the inner and outer labia, the head of the clitoris, the urethra, and the entrance to the vagina.
Images: Rayka Kumru
Sources
- Baytok, C. (2016). "'This isn't just about the bed, wait a minute!' Interview with Seven Kaptan", Part 2, Çatlak Zemin.
- Binik Y. M. (2010). The DSM diagnostic criteria for vaginismus. Archives of sexual behavior, 39(2), 278–291.
- Sex Education Research and Treatment Association (CETAD). (2006). “Information File - 1: Sexual Life and Its Problems”.
- Toothless, M., Mamuk, R., & Oskay, Ü. (2019). “Genito Pelvic Pain/Penetration Disorders and Current Approaches”, Journal of Düzce University Health Sciences Institute, 9(3): 202-208
- Omidvar Z., Bayazi M. H., & Faridhosseini F. (2021). Comparing the effectiveness of mindfulness-based cognitive therapy training and cognitive-behavioral therapy on sexual satisfaction of women with vaginismus disorder. Journal of Fundamentals of Mental Health, 267-271.
- The American Psychiatric Association (APA). (2013). Diagnostic and Statistical Manual of Mental Disorders, DSM-5, Fifth Edition.
- Vieira-Baptista, P., Lima-Silva, J., Pérez-López, F. R., Preti, M., & Bornstein, J. (2018). Vulvodynia: A disease commonly hidden in plain sight. Case reports in women's health, 20, e00079.